Having Trigeminal Neuralgia is painful and overwhelming and hard beyond the English language’s ability to describe it. Someone with TN, in my experience, often does not even try to really communicate the depth of the battle that it is, so I can certainly not explain it sufficiently.
If you child has Trigeminal Neuralgia, they are going through that fight on a daily basis. On top of that, kids have some unique, and incredibly frustrating challenges when facing this condition that is considered an “Over age 50” affliction.
Here we are going to discuss some of those challenges that need to be taken into consideration, and even expected at some level. As much as some of them will make you want to scream at someone, or hit something, we need to realize these things happen – and be ready to respond or compensate.
This is the first installment topic, more will follow.
Special Note: I reserve the right to modify, add to, and update this list going forward. It seems the longer we think and talk about this topic, the more things pop to mind.
.
Communication:
The most immediate and obvious issues will probably be communication. There is no test or scan that diagnoses Trigeminal Neuralgia, though many – even “top” doctors – will look to the MRI for compressions for diagnosis, MRIs are NOT effective at diagnosing TN. There are many facial and head pain conditions, so a proper diagnosis depends on an accurate description of the pain and any other symptoms, by a doctor with a large amount of knowledge and experience with Trigeminal Neuralgia. Depending on the age of your child, this can be anywhere from easily misunderstood to impossible.
Our daughter was 11 years old and highly verbal at the onset of symptoms. (Seriously, when she was very young one of her punishments was “no talking” for a short period of time. Within a minute she would be moaning in frustration at her lack of expression.) However, when we made it to the pediatrician, she kept using the word “headache” which threw things off for a short time, giving us a diagnosis of Atypical Migraine. Once we started keeping a detailed pain journal, and asking her to point to where it hurt, the discussion changed. But in her defense, she explained, “your face is part of your head, right?”
Very young children may not be verbal enough, or have a sufficient vocabulary to describe what they are feeling beyond the obvious pain. For the very young it will be important for you to pay careful attention to nonverbal communication. Are they holding a specific spot during pain? Are they pulling or pressing on a specific spot on their face or head? Are there things they have stopped doing – like eating, chewing (altogether or on a specific side), drinking cold beverages, brushing teeth.
Older children may still not have the subtle variations in vocabulary to tell you they are feeling “electric shock” pain, or a “boring” pain, subtle differences that are important. They can answer your questions, so knowing what to ask becomes important. The 5th neurosurgeon we went to did the absolute best job of this. He would ask her about an aspect of her pain, letting her describe it. But then he would also give her options to choose from in describing the location, pain descriptors, any other sensory factors. Choosing the right word was often much easier than coming up with it out of her head – it’s just important to give a wide enough range of options so they don’t just choose something to give you an answer. Sometimes these options would also be a starting point for her to say “It’s kind of like that, but it does this, too.” This is how a good diagnosis happens.
Some pain descriptors you can ask about are: aching, boring, burning, cutting, dull, electric, freezing, gnawing, inflamed, irritating, numbing, pins and needles, radiating, sharp, shocking, shooting, stabbing, stinging, tender, tight, tingling, throbbing, and vise-like. This is just a start, feel free to add your own.
Two tools that may help are:
A face front/side image you child can use to specifically point out where pain is located:
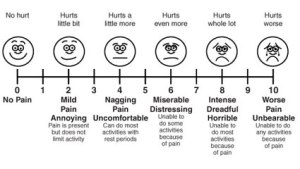
A photo of the 1-10 pain scale with some descriptors to help understand it:
It is also good to choose your times to ask about the pain. I would often ask limited questions during the pain when it wasn’t too bad. As the pain ramps up, there is no sense trying to ask annoying questions. However, often, an hour or so after the pain stopped, when my girl had rested, she would then be willing and able to answer my questions more thoroughly. It’s trial and error. See when it works to talk to your child. Experiment with different descriptors and see if any of them really connect with your child’s pain.
Your kid may do really well describing what they are going through. Or they may really struggle. Or, like mine, you may think they are doing great when you are actually missing important pieces. Know that we all miss things, we all stumble our way along. Especially in the beginning, but even throughout the journey. It’s ok. We offer this information to help, not to beat yourself up about – so you are now officially not allowed to do that.
Love, Hugs & Hope, from all of us to you.
This is a great article. We just met with dr ghosh this morning for a nerve block. He asked questions just like this, allowing her to describe than giving her options, He is our first neuro – so grateful to have found him.
LikeLike
He sounds like a good neuro – which is awesome! Wish you the best of luck with him, and that he is able to find a way to give your baby relief. Thank you for the encouragement on the article. 🙂 We keep talking about the information we wish we had had at the outset, to make our journey easier. Then we try to share it with all of you. Hugs & Hope to you!
LikeLike